cancer detection
Cancer detection using Artificial Intelligence (AI) involves leveraging advanced machine learning algorithms and techniques to identify and diagnose cancer from various medical data sources. The goal is to enhance early detection, improve diagnostic accuracy, and potentially reduce the need for invasive procedures.
Papers and Code
An Inclusive Foundation Model for Generalizable Cytogenetics in Precision Oncology
May 21, 2025Chromosome analysis is vital for diagnosing genetic disorders and guiding cancer therapy decisions through the identification of somatic clonal aberrations. However, developing an AI model are hindered by the overwhelming complexity and diversity of chromosomal abnormalities, requiring extensive annotation efforts, while automated methods remain task-specific and lack generalizability due to the scarcity of comprehensive datasets spanning diverse resource conditions. Here, we introduce CHROMA, a foundation model for cytogenomics, designed to overcome these challenges by learning generalizable representations of chromosomal abnormalities. Pre-trained on over 84,000 specimens (~4 million chromosomal images) via self-supervised learning, CHROMA outperforms other methods across all types of abnormalities, even when trained on fewer labelled data and more imbalanced datasets. By facilitating comprehensive mapping of instability and clonal leisons across various aberration types, CHROMA offers a scalable and generalizable solution for reliable and automated clinical analysis, reducing the annotation workload for experts and advancing precision oncology through the early detection of rare genomic abnormalities, enabling broad clinical AI applications and making advanced genomic analysis more accessible.
Automated Quality Evaluation of Cervical Cytopathology Whole Slide Images Based on Content Analysis
May 20, 2025The ThinPrep Cytologic Test (TCT) is the most widely used method for cervical cancer screening, and the sample quality directly impacts the accuracy of the diagnosis. Traditional manual evaluation methods rely on the observation of pathologist under microscopes. These methods exhibit high subjectivity, high cost, long duration, and low reliability. With the development of computer-aided diagnosis (CAD), an automated quality assessment system that performs at the level of a professional pathologist is necessary. To address this need, we propose a fully automated quality assessment method for Cervical Cytopathology Whole Slide Images (WSIs) based on The Bethesda System (TBS) diagnostic standards, artificial intelligence algorithms, and the characteristics of clinical data. The method analysis the context of WSIs to quantify quality evaluation metrics which are focused by TBS such as staining quality, cell counts and cell mass proportion through multiple models including object detection, classification and segmentation. Subsequently, the XGBoost model is used to mine the attention paid by pathologists to different quality evaluation metrics when evaluating samples, thereby obtaining a comprehensive WSI sample score calculation model. Experimental results on 100 WSIs demonstrate that the proposed evaluation method has significant advantages in terms of speed and consistency.
TransST: Transfer Learning Embedded Spatial Factor Modeling of Spatial Transcriptomics Data
Apr 15, 2025
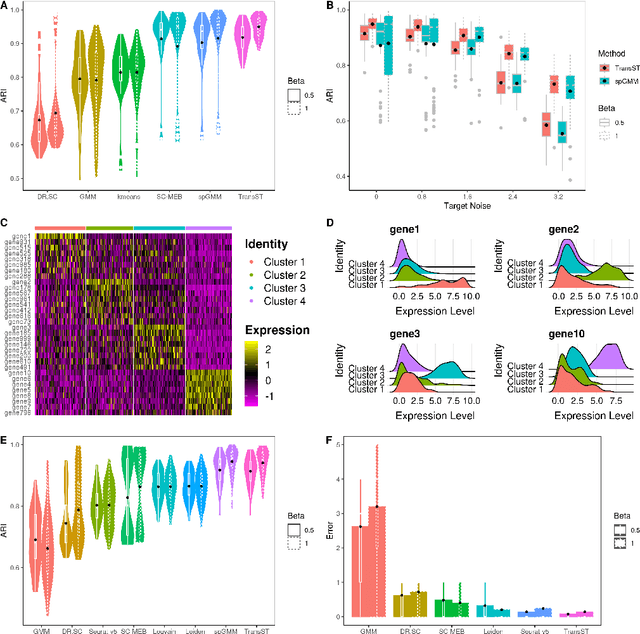


Background: Spatial transcriptomics have emerged as a powerful tool in biomedical research because of its ability to capture both the spatial contexts and abundance of the complete RNA transcript profile in organs of interest. However, limitations of the technology such as the relatively low resolution and comparatively insufficient sequencing depth make it difficult to reliably extract real biological signals from these data. To alleviate this challenge, we propose a novel transfer learning framework, referred to as TransST, to adaptively leverage the cell-labeled information from external sources in inferring cell-level heterogeneity of a target spatial transcriptomics data. Results: Applications in several real studies as well as a number of simulation settings show that our approach significantly improves existing techniques. For example, in the breast cancer study, TransST successfully identifies five biologically meaningful cell clusters, including the two subgroups of cancer in situ and invasive cancer; in addition, only TransST is able to separate the adipose tissues from the connective issues among all the studied methods. Conclusions: In summary, the proposed method TransST is both effective and robust in identifying cell subclusters and detecting corresponding driving biomarkers in spatial transcriptomics data.
Graph Kolmogorov-Arnold Networks for Multi-Cancer Classification and Biomarker Identification, An Interpretable Multi-Omics Approach
Mar 29, 2025The integration of multi-omics data presents a major challenge in precision medicine, requiring advanced computational methods for accurate disease classification and biological interpretation. This study introduces the Multi-Omics Graph Kolmogorov-Arnold Network (MOGKAN), a deep learning model that integrates messenger RNA, micro RNA sequences, and DNA methylation data with Protein-Protein Interaction (PPI) networks for accurate and interpretable cancer classification across 31 cancer types. MOGKAN employs a hybrid approach combining differential expression with DESeq2, Linear Models for Microarray (LIMMA), and Least Absolute Shrinkage and Selection Operator (LASSO) regression to reduce multi-omics data dimensionality while preserving relevant biological features. The model architecture is based on the Kolmogorov-Arnold theorem principle, using trainable univariate functions to enhance interpretability and feature analysis. MOGKAN achieves classification accuracy of 96.28 percent and demonstrates low experimental variability with a standard deviation that is reduced by 1.58 to 7.30 percents compared to Convolutional Neural Networks (CNNs) and Graph Neural Networks (GNNs). The biomarkers identified by MOGKAN have been validated as cancer-related markers through Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis. The proposed model presents an ability to uncover molecular oncogenesis mechanisms by detecting phosphoinositide-binding substances and regulating sphingolipid cellular processes. By integrating multi-omics data with graph-based deep learning, our proposed approach demonstrates superior predictive performance and interpretability that has the potential to enhance the translation of complex multi-omics data into clinically actionable cancer diagnostics.
Single Shot AI-assisted quantification of KI-67 proliferation index in breast cancer
Mar 25, 2025Reliable quantification of Ki-67, a key proliferation marker in breast cancer, is essential for molecular subtyping and informed treatment planning. Conventional approaches, including visual estimation and manual counting, suffer from interobserver variability and limited reproducibility. This study introduces an AI-assisted method using the YOLOv8 object detection framework for automated Ki-67 scoring. High-resolution digital images (40x magnification) of immunohistochemically stained tumor sections were captured from Ki-67 hotspot regions and manually annotated by a domain expert to distinguish Ki-67-positive and negative tumor cells. The dataset was augmented and divided into training (80%), validation (10%), and testing (10%) subsets. Among the YOLOv8 variants tested, the Medium model achieved the highest performance, with a mean Average Precision at 50% Intersection over Union (mAP50) exceeding 85% for Ki-67-positive cells. The proposed approach offers an efficient, scalable, and objective alternative to conventional scoring methods, supporting greater consistency in Ki-67 evaluation. Future directions include developing user-friendly clinical interfaces and expanding to multi-institutional datasets to enhance generalizability and facilitate broader adoption in diagnostic practice.
Tumor monitoring and detection of lymph node metastasis using quantitative ultrasound and immune cytokine profiling in dogs undergoing radiation therapy: a pilot study
Mar 25, 2025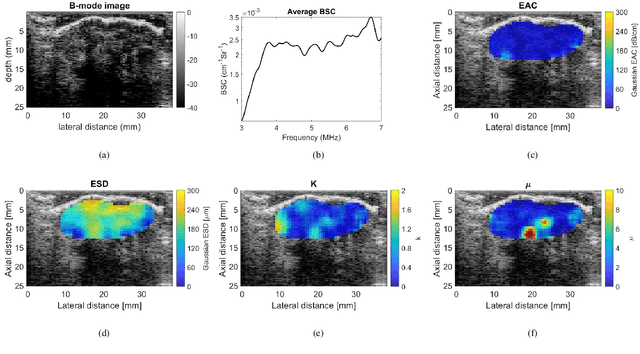
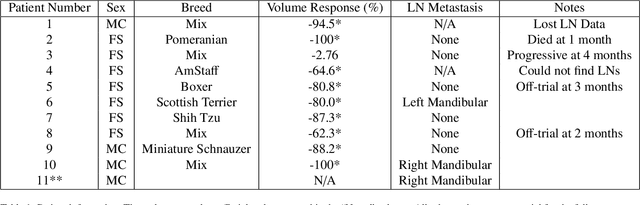
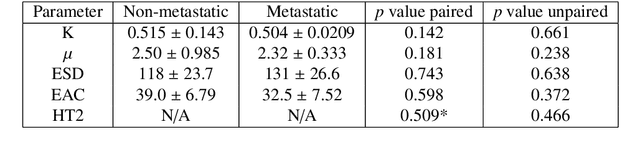
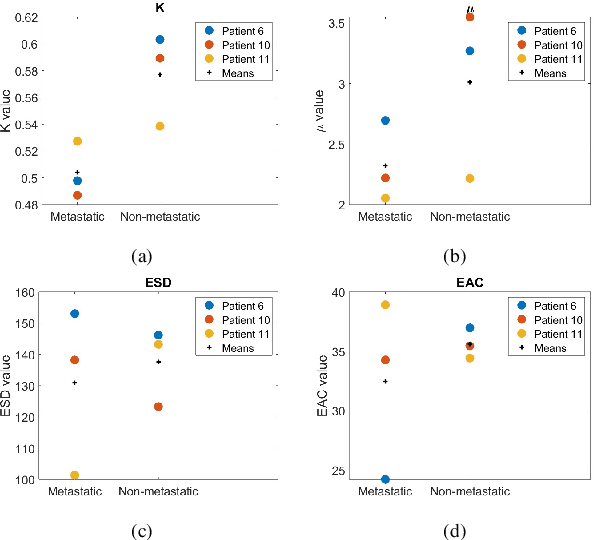
Quantitative ultrasound (QUS) characterizes the composition of cells to distinguish diseased from healthy tissue. QUS can reflect the complexity of the tumor and detect early lymph node (LN) metastasis ex vivo. The objective in this study was to gather preliminary QUS and cytokine data from dogs undergoing radiation therapy and correlate QUS data with both LN metastasis and tumor response. Spontaneous solid tumors were evaluated with QUS before and up to one year after receiving RT. Additionally, regional LNs were evaluated with QUS in vivo, then excised and examined with histopathology to detect metastasis. Paired t-tests were used to compare QUS data of metastatic and non-metastatic LNs within patients. Furthermore, paired t-tests compared pre- versus post-RT QUS data. Serum was collected at each time point for cytokine profiles. Most statistical tests were underpowered to produce significant p values, but interesting trends were observed. The lowest p values for LN tests were found with the envelope statistics K (p = 0.142) and mu (p = 0.181), which correspond to cell structure and number of scatterers. For tumor response, the lowest p values were found with K (p = 0.115) and mu (p = 0.127) when comparing baseline QUS data with QUS data 1 week after RT. Monocyte chemoattractant protein 1 (MCP-1) was significantly higher in dogs with cancer when compared to healthy controls (p = 1.12e-4). A weak correlation was found between effective scatterer diameter (ESD) and Transforming growth factor beta 1 (TGFB-1). While statistical tests on the preliminary QUS data alone were underpowered to detect significant differences among groups, our methods create a basis for future studies.
SMILE: a Scale-aware Multiple Instance Learning Method for Multicenter STAS Lung Cancer Histopathology Diagnosis
Mar 18, 2025Spread through air spaces (STAS) represents a newly identified aggressive pattern in lung cancer, which is known to be associated with adverse prognostic factors and complex pathological features. Pathologists currently rely on time consuming manual assessments, which are highly subjective and prone to variation. This highlights the urgent need for automated and precise diag nostic solutions. 2,970 lung cancer tissue slides are comprised from multiple centers, re-diagnosed them, and constructed and publicly released three lung cancer STAS datasets: STAS CSU (hospital), STAS TCGA, and STAS CPTAC. All STAS datasets provide corresponding pathological feature diagnoses and related clinical data. To address the bias, sparse and heterogeneous nature of STAS, we propose an scale-aware multiple instance learning(SMILE) method for STAS diagnosis of lung cancer. By introducing a scale-adaptive attention mechanism, the SMILE can adaptively adjust high attention instances, reducing over-reliance on local regions and promoting consistent detection of STAS lesions. Extensive experiments show that SMILE achieved competitive diagnostic results on STAS CSU, diagnosing 251 and 319 STAS samples in CPTAC andTCGA,respectively, surpassing clinical average AUC. The 11 open baseline results are the first to be established for STAS research, laying the foundation for the future expansion, interpretability, and clinical integration of computational pathology technologies. The datasets and code are available at https://anonymous.4open.science/r/IJCAI25-1DA1.
Leveraging Sparse Annotations for Leukemia Diagnosis on the Large Leukemia Dataset
Apr 03, 2025Leukemia is 10th most frequently diagnosed cancer and one of the leading causes of cancer related deaths worldwide. Realistic analysis of Leukemia requires White Blook Cells (WBC) localization, classification, and morphological assessment. Despite deep learning advances in medical imaging, leukemia analysis lacks a large, diverse multi-task dataset, while existing small datasets lack domain diversity, limiting real world applicability. To overcome dataset challenges, we present a large scale WBC dataset named Large Leukemia Dataset (LLD) and novel methods for detecting WBC with their attributes. Our contribution here is threefold. First, we present a large-scale Leukemia dataset collected through Peripheral Blood Films (PBF) from several patients, through multiple microscopes, multi cameras, and multi magnification. To enhance diagnosis explainability and medical expert acceptance, each leukemia cell is annotated at 100x with 7 morphological attributes, ranging from Cell Size to Nuclear Shape. Secondly, we propose a multi task model that not only detects WBCs but also predicts their attributes, providing an interpretable and clinically meaningful solution. Third, we propose a method for WBC detection with attribute analysis using sparse annotations. This approach reduces the annotation burden on hematologists, requiring them to mark only a small area within the field of view. Our method enables the model to leverage the entire field of view rather than just the annotated regions, enhancing learning efficiency and diagnostic accuracy. From diagnosis explainability to overcoming domain shift challenges, presented datasets could be used for many challenging aspects of microscopic image analysis. The datasets, code, and demo are available at: https://im.itu.edu.pk/sparse-leukemiaattri/
Efficient Brain Tumor Segmentation Using a Dual-Decoder 3D U-Net with Attention Gates (DDUNet)
Apr 14, 2025



Cancer remains one of the leading causes of mortality worldwide, and among its many forms, brain tumors are particularly notorious due to their aggressive nature and the critical challenges involved in early diagnosis. Recent advances in artificial intelligence have shown great promise in assisting medical professionals with precise tumor segmentation, a key step in timely diagnosis and treatment planning. However, many state-of-the-art segmentation methods require extensive computational resources and prolonged training times, limiting their practical application in resource-constrained settings. In this work, we present a novel dual-decoder U-Net architecture enhanced with attention-gated skip connections, designed specifically for brain tumor segmentation from MRI scans. Our approach balances efficiency and accuracy by achieving competitive segmentation performance while significantly reducing training demands. Evaluated on the BraTS 2020 dataset, the proposed model achieved Dice scores of 85.06% for Whole Tumor (WT), 80.61% for Tumor Core (TC), and 71.26% for Enhancing Tumor (ET) in only 50 epochs, surpassing several commonly used U-Net variants. Our model demonstrates that high-quality brain tumor segmentation is attainable even under limited computational resources, thereby offering a viable solution for researchers and clinicians operating with modest hardware. This resource-efficient model has the potential to improve early detection and diagnosis of brain tumors, ultimately contributing to better patient outcomes
SCFANet: Style Distribution Constraint Feature Alignment Network For Pathological Staining Translation
Apr 01, 2025



Immunohistochemical (IHC) staining serves as a valuable technique for detecting specific antigens or proteins through antibody-mediated visualization. However, the IHC staining process is both time-consuming and costly. To address these limitations, the application of deep learning models for direct translation of cost-effective Hematoxylin and Eosin (H&E) stained images into IHC stained images has emerged as an efficient solution. Nevertheless, the conversion from H&E to IHC images presents significant challenges, primarily due to alignment discrepancies between image pairs and the inherent diversity in IHC staining style patterns. To overcome these challenges, we propose the Style Distribution Constraint Feature Alignment Network (SCFANet), which incorporates two innovative modules: the Style Distribution Constrainer (SDC) and Feature Alignment Learning (FAL). The SDC ensures consistency between the generated and target images' style distributions while integrating cycle consistency loss to maintain structural consistency. To mitigate the complexity of direct image-to-image translation, the FAL module decomposes the end-to-end translation task into two subtasks: image reconstruction and feature alignment. Furthermore, we ensure pathological consistency between generated and target images by maintaining pathological pattern consistency and Optical Density (OD) uniformity. Extensive experiments conducted on the Breast Cancer Immunohistochemical (BCI) dataset demonstrate that our SCFANet model outperforms existing methods, achieving precise transformation of H&E-stained images into their IHC-stained counterparts. The proposed approach not only addresses the technical challenges in H&E to IHC image translation but also provides a robust framework for accurate and efficient stain conversion in pathological analysis.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge