Yi-han Sheu
Massachusetts General Hospital, Boston, MA
Large Language Models in Mental Health Care: a Scoping Review
Jan 01, 2024



Abstract:Objective: The growing use of large language models (LLMs) stimulates a need for a comprehensive review of their applications and outcomes in mental health care contexts. This scoping review aims to critically analyze the existing development and applications of LLMs in mental health care, highlighting their successes and identifying their challenges and limitations in these specialized fields. Materials and Methods: A broad literature search was conducted in November 2023 using six databases (PubMed, Web of Science, Google Scholar, arXiv, medRxiv, and PsyArXiv) following the 2020 version of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A total of 313 publications were initially identified, and after applying the study inclusion criteria, 34 publications were selected for the final review. Results: We identified diverse applications of LLMs in mental health care, including diagnosis, therapy, patient engagement enhancement, etc. Key challenges include data availability and reliability, nuanced handling of mental states, and effective evaluation methods. Despite successes in accuracy and accessibility improvement, gaps in clinical applicability and ethical considerations were evident, pointing to the need for robust data, standardized evaluations, and interdisciplinary collaboration. Conclusion: LLMs show promising potential in advancing mental health care, with applications in diagnostics, and patient support. Continued advancements depend on collaborative, multidisciplinary efforts focused on framework enhancement, rigorous dataset development, technological refinement, and ethical integration to ensure the effective and safe application of LLMs in mental health care.
Using Deep Learning to Identify Patients with Cognitive Impairment in Electronic Health Records
Nov 13, 2021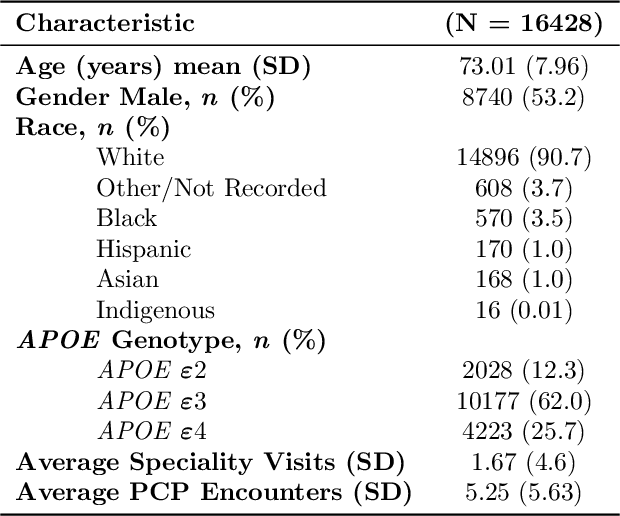

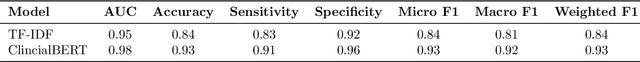

Abstract:Dementia is a neurodegenerative disorder that causes cognitive decline and affects more than 50 million people worldwide. Dementia is under-diagnosed by healthcare professionals - only one in four people who suffer from dementia are diagnosed. Even when a diagnosis is made, it may not be entered as a structured International Classification of Diseases (ICD) diagnosis code in a patient's charts. Information relevant to cognitive impairment (CI) is often found within electronic health records (EHR), but manual review of clinician notes by experts is both time consuming and often prone to errors. Automated mining of these notes presents an opportunity to label patients with cognitive impairment in EHR data. We developed natural language processing (NLP) tools to identify patients with cognitive impairment and demonstrate that linguistic context enhances performance for the cognitive impairment classification task. We fine-tuned our attention based deep learning model, which can learn from complex language structures, and substantially improved accuracy (0.93) relative to a baseline NLP model (0.84). Further, we show that deep learning NLP can successfully identify dementia patients without dementia-related ICD codes or medications.
Natural Language Processing to Detect Cognitive Concerns in Electronic Health Records Using Deep Learning
Nov 12, 2020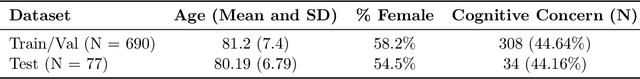
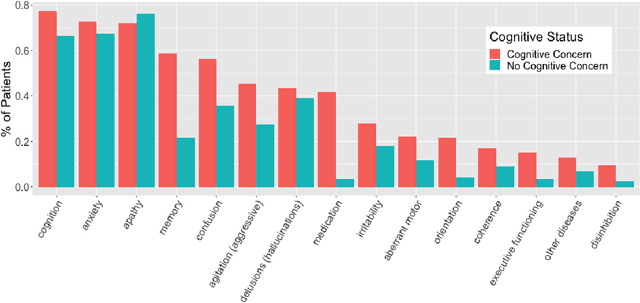
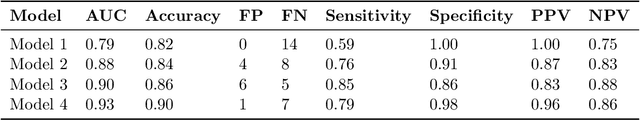
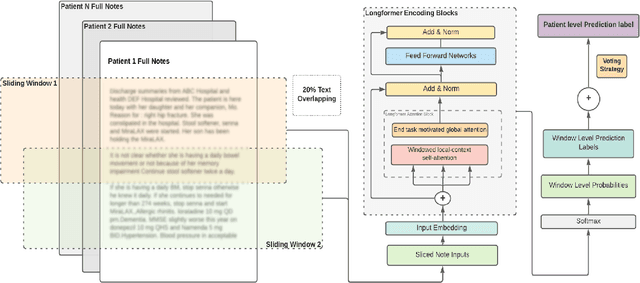
Abstract:Dementia is under-recognized in the community, under-diagnosed by healthcare professionals, and under-coded in claims data. Information on cognitive dysfunction, however, is often found in unstructured clinician notes within medical records but manual review by experts is time consuming and often prone to errors. Automated mining of these notes presents a potential opportunity to label patients with cognitive concerns who could benefit from an evaluation or be referred to specialist care. In order to identify patients with cognitive concerns in electronic medical records, we applied natural language processing (NLP) algorithms and compared model performance to a baseline model that used structured diagnosis codes and medication data only. An attention-based deep learning model outperformed the baseline model and other simpler models.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge