Ibraheem Hamdi
Foundation Models in Biomedical Imaging: Turning Hype into Reality
Dec 17, 2025



Abstract:Foundation models (FMs) are driving a prominent shift in artificial intelligence across different domains, including biomedical imaging. These models are designed to move beyond narrow pattern recognition towards emulating sophisticated clinical reasoning, understanding complex spatial relationships, and integrating multimodal data with unprecedented flexibility. However, a critical gap exists between this potential and the current reality, where the clinical evaluation and deployment of FMs are hampered by significant challenges. Herein, we critically assess the current state-of-the-art, analyzing hype by examining the core capabilities and limitations of FMs in the biomedical domain. We also provide a taxonomy of reasoning, ranging from emulated sequential logic and spatial understanding to the integration of explicit symbolic knowledge, to evaluate whether these models exhibit genuine cognition or merely mimic surface-level patterns. We argue that a critical frontier lies beyond statistical correlation, in the pursuit of causal inference, which is essential for building robust models that understand cause and effect. Furthermore, we discuss the paramount issues in deployment stemming from trustworthiness, bias, and safety, dissecting the challenges of algorithmic bias, data bias and privacy, and model hallucinations. We also draw attention to the need for more inclusive, rigorous, and clinically relevant validation frameworks to ensure their safe and ethical application. We conclude that while the vision of autonomous AI-doctors remains distant, the immediate reality is the emergence of powerful technology and assistive tools that would benefit clinical practice. The future of FMs in biomedical imaging hinges not on scale alone, but on developing hybrid, causally aware, and verifiably safe systems that augment, rather than replace, human expertise.
Hyperparameter Optimization for COVID-19 Chest X-Ray Classification
Jan 26, 2022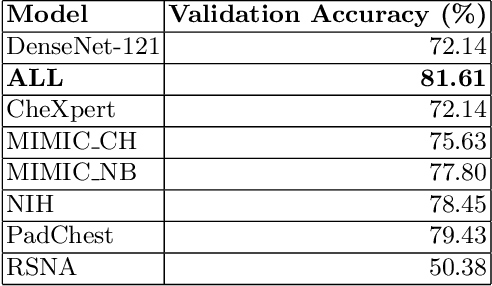
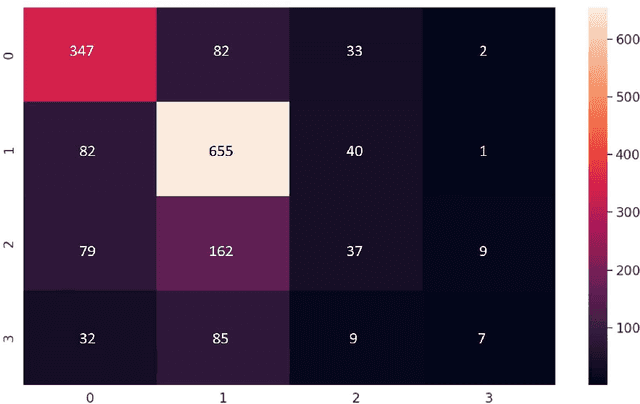
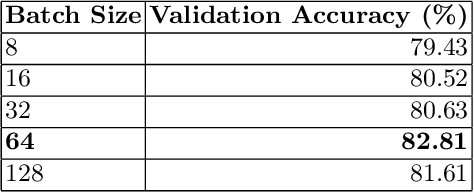
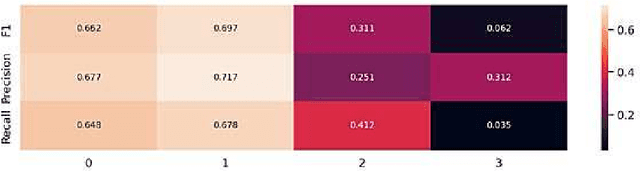
Abstract:Despite the introduction of vaccines, Coronavirus disease (COVID-19) remains a worldwide dilemma, continuously developing new variants such as Delta and the recent Omicron. The current standard for testing is through polymerase chain reaction (PCR). However, PCRs can be expensive, slow, and/or inaccessible to many people. X-rays on the other hand have been readily used since the early 20th century and are relatively cheaper, quicker to obtain, and typically covered by health insurance. With a careful selection of model, hyperparameters, and augmentations, we show that it is possible to develop models with 83% accuracy in binary classification and 64% in multi-class for detecting COVID-19 infections from chest x-rays.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge