Carlos Cardenas
Virtual Dosimetrists: A Radiotherapy Training "Flight Simulator"
May 14, 2025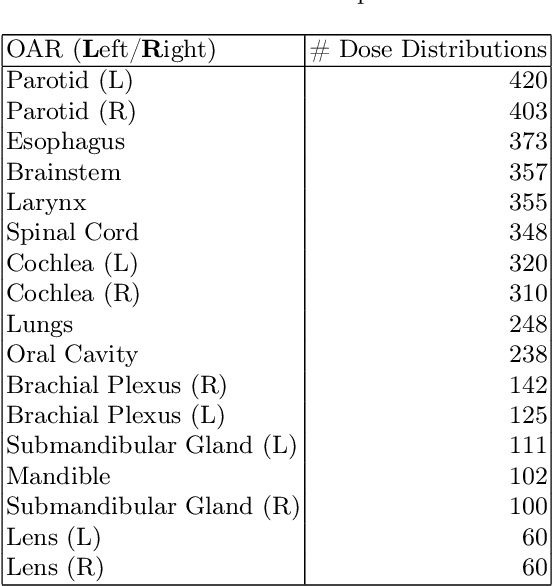


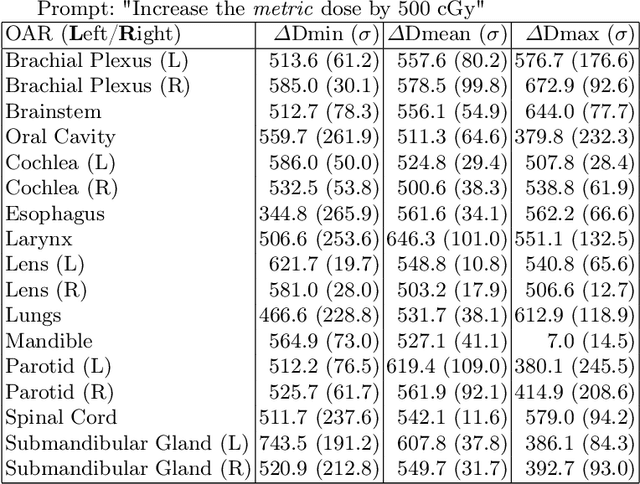
Abstract:Effective education in radiotherapy plan quality review requires a robust, regularly updated set of examples and the flexibility to demonstrate multiple possible planning approaches and their consequences. However, the current clinic-based paradigm does not support these needs. To address this, we have developed 'Virtual Dosimetrist' models that can both generate training examples of suboptimal treatment plans and then allow trainees to improve the plan quality through simple natural language prompts, as if communicating with a dosimetrist. The dose generation and modification process is accurate, rapid, and requires only modest resources. This work is the first to combine dose distribution prediction with natural language processing; providing a robust pipeline for both generating suboptimal training plans and allowing trainees to practice their critical plan review and improvement skills that addresses the challenges of the current clinic-based paradigm.
Automated WBRT Treatment Planning via Deep Learning Auto-Contouring and Customizable Landmark-Based Field Aperture Design
May 24, 2022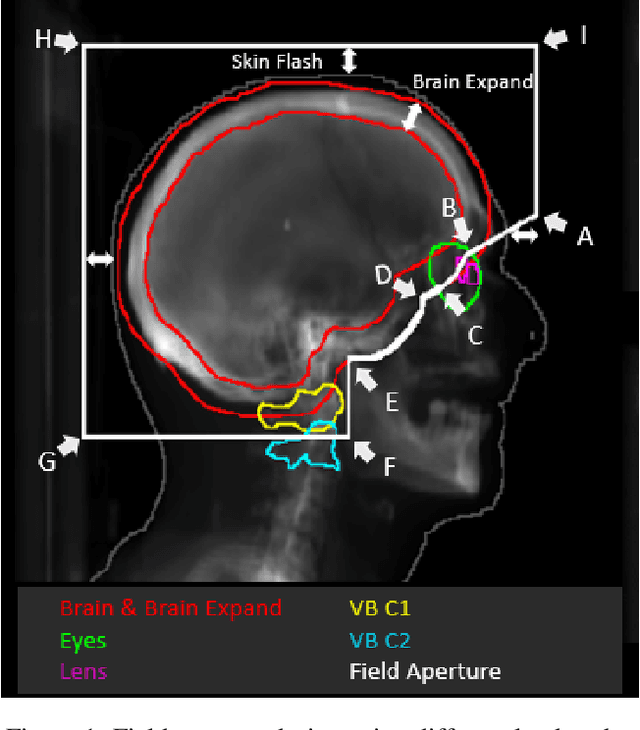
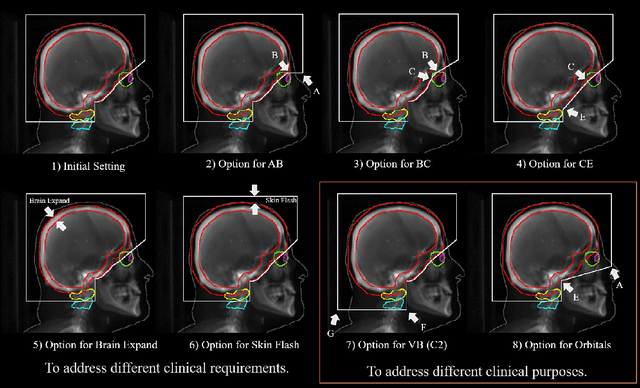
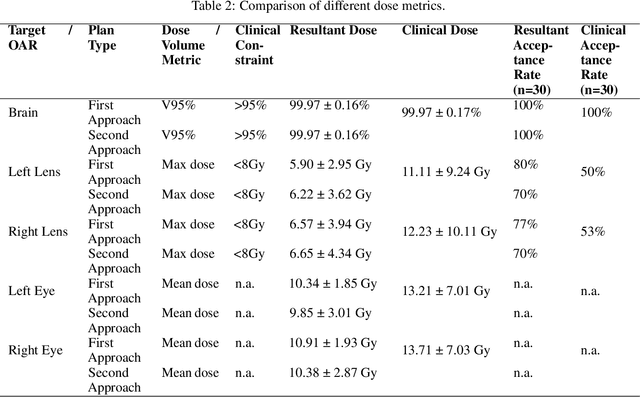
Abstract:In this work, we developed and evaluated a novel pipeline consisting of two landmark-based field aperture generation approaches for WBRT treatment planning; they are fully automated and customizable. The automation pipeline is beneficial for both clinicians and patients, where we can reduce clinician workload and reduce treatment planning time. The customizability of the field aperture design addresses different clinical requirements and allows the personalized design to become feasible. The performance results regarding quantitative and qualitative evaluations demonstrated that our plans were comparable with the original clinical plans. This technique has been deployed as part of a fully automated treatment planning tool for whole-brain cancer and could be translated to other treatment sites in the future.
Automation of Radiation Treatment Planning for Rectal Cancer
Apr 26, 2022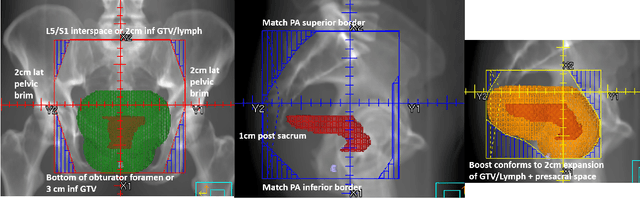
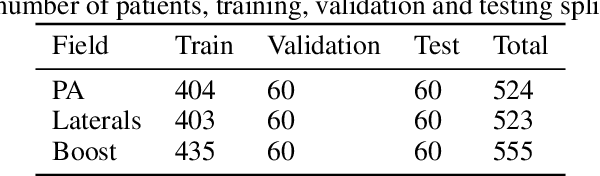
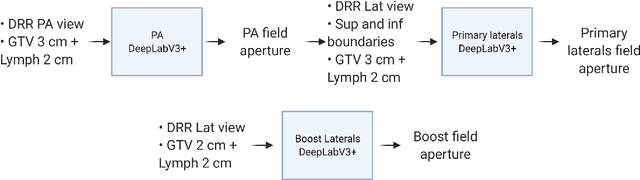
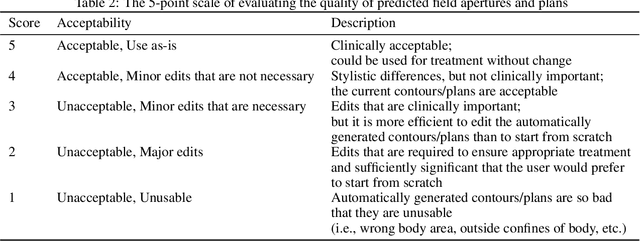
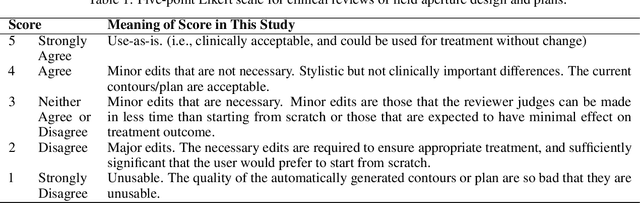
Abstract:To develop an automated workflow for rectal cancer three-dimensional conformal radiotherapy treatment planning that combines deep-learning(DL) aperture predictions and forward-planning algorithms. We designed an algorithm to automate the clinical workflow for planning with field-in-field. DL models were trained, validated, and tested on 555 patients to automatically generate aperture shapes for primary and boost fields. Network inputs were digitally reconstructed radiography, gross tumor volume(GTV), and nodal GTV. A physician scored each aperture for 20 patients on a 5-point scale(>3 acceptable). A planning algorithm was then developed to create a homogeneous dose using a combination of wedges and subfields. The algorithm iteratively identifies a hotspot volume, creates a subfield, and optimizes beam weight all without user intervention. The algorithm was tested on 20 patients using clinical apertures with different settings, and the resulting plans(4 plans/patient) were scored by a physician. The end-to-end workflow was tested and scored by a physician on 39 patients using DL-generated apertures and planning algorithms. The predicted apertures had Dice scores of 0.95, 0.94, and 0.90 for posterior-anterior, laterals, and boost fields, respectively. 100%, 95%, and 87.5% of the posterior-anterior, laterals, and boost apertures were scored as clinically acceptable, respectively. Wedged and non-wedged plans were clinically acceptable for 85% and 50% of patients, respectively. The final plans hotspot dose percentage was reduced from 121%($\pm$ 14%) to 109%($\pm$ 5%) of prescription dose. The integrated end-to-end workflow of automatically generated apertures and optimized field-in-field planning gave clinically acceptable plans for 38/39(97%) of patients. We have successfully automated the clinical workflow for generating radiotherapy plans for rectal cancer for our institution.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge