Jiwoong Jeong
MOSCARD -- Causal Reasoning and De-confounding for Multimodal Opportunistic Screening of Cardiovascular Adverse Events
Jun 23, 2025



Abstract:Major Adverse Cardiovascular Events (MACE) remain the leading cause of mortality globally, as reported in the Global Disease Burden Study 2021. Opportunistic screening leverages data collected from routine health check-ups and multimodal data can play a key role to identify at-risk individuals. Chest X-rays (CXR) provide insights into chronic conditions contributing to major adverse cardiovascular events (MACE), while 12-lead electrocardiogram (ECG) directly assesses cardiac electrical activity and structural abnormalities. Integrating CXR and ECG could offer a more comprehensive risk assessment than conventional models, which rely on clinical scores, computed tomography (CT) measurements, or biomarkers, which may be limited by sampling bias and single modality constraints. We propose a novel predictive modeling framework - MOSCARD, multimodal causal reasoning with co-attention to align two distinct modalities and simultaneously mitigate bias and confounders in opportunistic risk estimation. Primary technical contributions are - (i) multimodal alignment of CXR with ECG guidance; (ii) integration of causal reasoning; (iii) dual back-propagation graph for de-confounding. Evaluated on internal, shift data from emergency department (ED) and external MIMIC datasets, our model outperformed single modality and state-of-the-art foundational models - AUC: 0.75, 0.83, 0.71 respectively. Proposed cost-effective opportunistic screening enables early intervention, improving patient outcomes and reducing disparities.
Was there COVID-19 back in 2012? Challenge for AI in Diagnosis with Similar Indications
Jun 23, 2020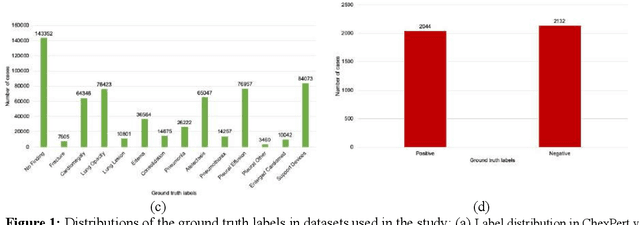
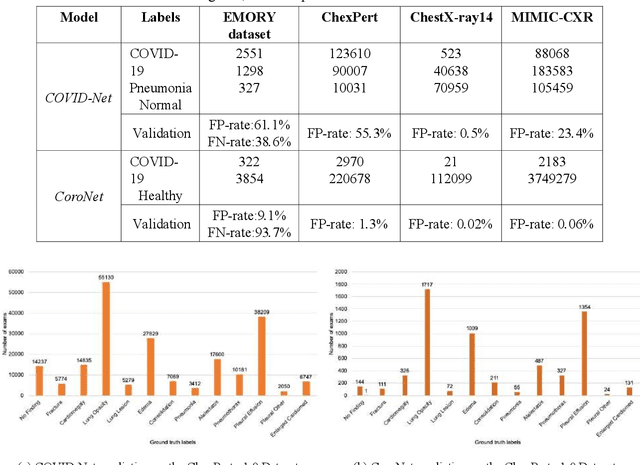
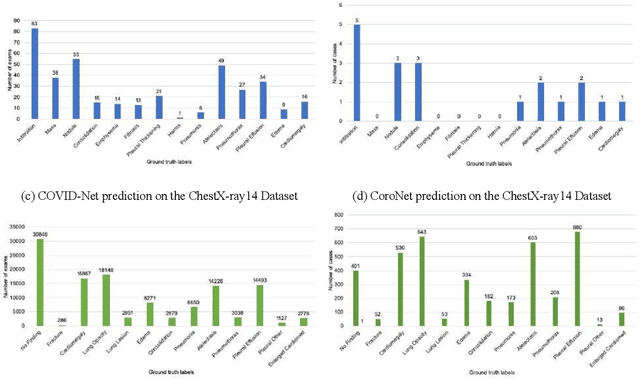
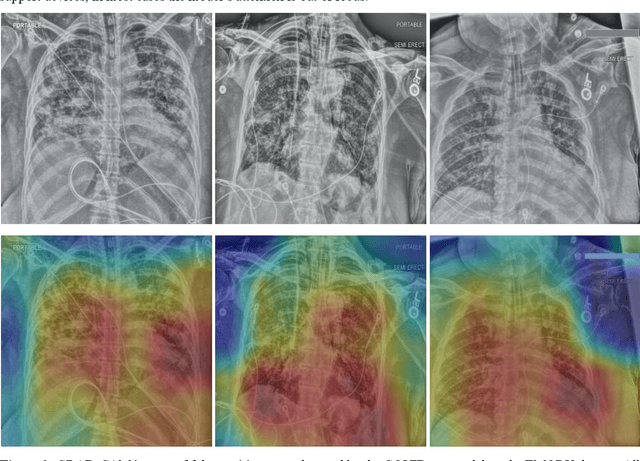
Abstract:Purpose: Since the recent COVID-19 outbreak, there has been an avalanche of research papers applying deep learning based image processing to chest radiographs for detection of the disease. To test the performance of the two top models for CXR COVID-19 diagnosis on external datasets to assess model generalizability. Methods: In this paper, we present our argument regarding the efficiency and applicability of existing deep learning models for COVID-19 diagnosis. We provide results from two popular models - COVID-Net and CoroNet evaluated on three publicly available datasets and an additional institutional dataset collected from EMORY Hospital between January and May 2020, containing patients tested for COVID-19 infection using RT-PCR. Results: There is a large false positive rate (FPR) for COVID-Net on both ChexPert (55.3%) and MIMIC-CXR (23.4%) dataset. On the EMORY Dataset, COVID-Net has 61.4% sensitivity, 0.54 F1-score and 0.49 precision value. The FPR of the CoroNet model is significantly lower across all the datasets as compared to COVID-Net - EMORY(9.1%), ChexPert (1.3%), ChestX-ray14 (0.02%), MIMIC-CXR (0.06%). Conclusion: The models reported good to excellent performance on their internal datasets, however we observed from our testing that their performance dramatically worsened on external data. This is likely from several causes including overfitting models due to lack of appropriate control patients and ground truth labels. The fourth institutional dataset was labeled using RT-PCR, which could be positive without radiographic findings and vice versa. Therefore, a fusion model of both clinical and radiographic data may have better performance and generalization.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge